Leads ECG Placement: 7 Critical Mistakes You Must Avoid Now
Understanding leads ecg placement is essential for accurate cardiac diagnostics. A simple error in electrode positioning can lead to misdiagnosis, delayed treatment, or unnecessary interventions. In this comprehensive guide, we’ll explore everything you need to know to master proper leads ecg placement—backed by clinical evidence and expert insights.
What Is Leads ECG Placement and Why It Matters

Leads ecg placement refers to the precise positioning of electrodes on the body to record the heart’s electrical activity. The 12-lead ECG, the gold standard in cardiac assessment, relies on accurate electrode placement to generate reliable data. Misplacement, even by a few centimeters, can distort waveforms and mimic pathologies like myocardial infarction or arrhythmias.
Anatomy of a 12-Lead ECG System
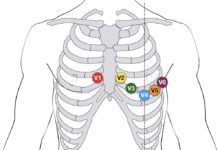
The 12-lead ECG uses 10 electrodes to produce 12 different electrical views (leads) of the heart. These leads are divided into limb leads (I, II, III, aVR, aVL, aVF) and precordial (chest) leads (V1–V6). Each lead provides a unique angle of the heart’s electrical axis, enabling clinicians to localize ischemia, infarction, or conduction abnormalities.
- Limb leads: Derived from electrodes on the arms and legs.
- Precordial leads: Placed across the chest in specific intercostal spaces.
- Augmented leads: Use a combination of limb electrodes to enhance signal clarity.
According to the American Heart Association (AHA), standardized placement is critical for diagnostic consistency across settings and providers (American Heart Association).
Common Errors in Leads ECG Placement
Despite its routine use, incorrect leads ecg placement remains surprisingly common. Studies show up to 40% of ECGs have at least one electrode misplaced. The most frequent errors include:
- Swapping right and left arm electrodes, which reverses lead I and can mimic dextrocardia.
- Placing precordial leads too high or too lateral, altering R-wave progression.
- Incorrect intercostal space identification, especially in obese or elderly patients.
“A misplaced electrode can create an ECG pattern indistinguishable from acute coronary syndrome,” says Dr. Emily Tran, a cardiologist at Massachusetts General Hospital.
Step-by-Step Guide to Correct Leads ECG Placement
Performing a flawless ECG starts with meticulous attention to detail. Follow this step-by-step protocol to ensure accurate leads ecg placement every time.
Preparing the Patient and Equipment
Before placing any electrodes, ensure the patient is lying flat, relaxed, and warm. Cold or tense muscles can cause artifact interference. Expose the chest fully and clean the skin with alcohol wipes to reduce impedance. Shave excessive chest hair if necessary to ensure electrode adhesion.
- Use disposable, high-quality electrodes designed for ECG use.
- Check lead wires for damage or fraying.
- Ensure the ECG machine is calibrated and grounded properly.
Proper preparation minimizes noise and baseline wander, improving signal fidelity (NCBI ECG Guide).
Positioning the Limb Electrodes
Limb electrodes should be placed on the distal parts of the limbs—on the wrists and ankles—but not directly over joints. Avoid bony prominences and areas with muscle movement.
- RA (Right Arm): On the right wrist or upper forearm.
- LA (Left Arm): On the left wrist or upper forearm.
- RL (Right Leg): On the right ankle or lower leg (ground electrode).
- LL (Left Leg): On the left ankle or lower leg.
For ambulatory or stressed patients, electrodes can be placed on the upper arms and lower abdomen to reduce motion artifact, but this must be documented.
Placing the Precordial (Chest) Leads Accurately
The precordial leads (V1–V6) are the most vulnerable to misplacement. Use anatomical landmarks to locate each position precisely.
- V1: 4th intercostal space, right sternal border.
- V2: 4th intercostal space, left sternal border.
- V3: Midway between V2 and V4.
- V4: 5th intercostal space, midclavicular line.
- V5: Same horizontal level as V4, anterior axillary line.
- V6: Same level as V4, midaxillary line.
Incorrect V1/V2 placement is linked to false diagnosis of anterior MI. A study in the Journal of Electrocardiology found that even 1-inch displacement alters QRS amplitude significantly (Journal of Electrocardiology).
The Impact of Incorrect Leads ECG Placement on Diagnosis
Inaccurate leads ecg placement doesn’t just produce a messy tracing—it can lead to life-threatening diagnostic errors. The ECG is often the first tool used in emergency settings, and flawed data can cascade into inappropriate care.
Mimicking Myocardial Infarction
One of the most dangerous consequences of misplaced precordial leads is the false appearance of ST-segment elevation. For example, if V1 and V2 are placed too high (e.g., 2nd or 3rd intercostal space), the ECG may show exaggerated R waves and ST elevation, mimicking anterior STEMI.
- This can trigger unnecessary activation of the cath lab.
- Patients may receive thrombolytics or undergo angiography without indication.
- Healthcare costs and patient risk increase significantly.
A case report in Circulation described a patient who was nearly taken to the cath lab due to a misplaced V1 electrode (Circulation Journal).
Altering Axis and R-Wave Progression
Lead misplacement can shift the perceived electrical axis of the heart. Swapping left and right arm electrodes reverses the frontal plane axis, making it appear as if the heart is on the right side (dextrocardia).
- Incorrect V3–V6 placement disrupts R-wave progression, suggesting anterior infarction.
- Lateral lead misplacement may mask true lateral MI.
- These changes affect both acute diagnosis and long-term monitoring.
“We once had a patient diagnosed with a massive anterior MI. After rechecking, we found V1 was on the 2nd rib. The repeat ECG was normal,” recalls Dr. Alan Perez, ER physician.
Special Considerations in Leads ECG Placement
While standard guidelines apply to most adults, certain populations require modifications to ensure accurate leads ecg placement.
ECG in Women and Breast Tissue
One of the most debated topics in leads ecg placement is how to handle breast tissue in women. Electrodes must be placed on the chest wall, not on breast tissue, to avoid signal distortion.
- V3–V6 should be positioned on the chest wall beneath the breast, not on the breast itself.
- Lifting and supporting the breast during placement ensures correct anatomical positioning.
- Failure to do so can cause poor R-wave progression and mimic ischemia.
The AHA recommends that clinicians receive training in gender-sensitive ECG techniques to avoid diagnostic errors (AHA Professional Resources).
Obese and Elderly Patients
In obese patients, identifying intercostal spaces can be challenging due to adipose tissue. In the elderly, skin elasticity and anatomical changes (e.g., kyphosis) complicate landmark identification.
- Use palpation, not visual estimation, to locate the angle of Louis and rib spaces.
- Consider using ECG electrode guides or templates for consistency.
- Document any deviations from standard placement for future comparison.
A 2020 study in The American Journal of Emergency Medicine showed that using a palpation-based protocol reduced ECG errors by 60% in obese patients.
Pediatric and Neonatal Leads ECG Placement
Children have smaller thoraxes and different heart positions, requiring adjustments in leads ecg placement.
- Use pediatric-sized electrodes to prevent overlap and signal interference.
- Place V leads in the same anatomical positions but consider age-appropriate spacing.
- In neonates, V4R (right-sided V4) is often added to assess right ventricular function.
The American Academy of Pediatrics emphasizes standardized training for pediatric ECGs to prevent misinterpretation.
Technological Aids for Accurate Leads ECG Placement
As healthcare embraces digital innovation, several tools now assist in achieving correct leads ecg placement.
ECG Electrode Placement Guides and Templates
Reusable or disposable templates help standardize electrode positioning. These are especially useful in training settings or high-volume clinics.
- Templates are placed on the chest to mark V1–V6 locations.
- Some include limb lead indicators for full standardization.
- Studies show templates reduce inter-operator variability by up to 75%.
Hospitals using placement guides report fewer repeat ECGs and higher diagnostic confidence.
Digital ECG Systems with Real-Time Feedback
Modern ECG machines now offer real-time impedance checks and lead placement verification.
- Some systems alert the technician if electrode contact is poor.
- Advanced models use AI to detect likely misplacement based on waveform patterns.
- These systems integrate with electronic health records for quality tracking.
Philips and GE Healthcare have introduced smart ECG devices that flag potential placement errors before recording (Philips Healthcare).
Augmented Reality and Mobile Apps
Emerging technologies like AR apps project electrode positions onto the patient’s body using smartphone cameras.
- Apps like “ECG Guide AR” overlay correct lead positions in real time.
- Useful for student training and remote settings.
- Still in early adoption but show promise for reducing human error.
“Technology won’t replace skill, but it can support consistency,” says Dr. Lena Kim, a biomedical engineer at Stanford.
Training and Education for Proper Leads ECG Placement
Despite its importance, formal training in leads ecg placement is often inadequate in medical and nursing curricula.
Current Gaps in Clinical Training
Many healthcare providers learn ECG placement through observation rather than structured education. This leads to the propagation of incorrect techniques.
- Studies show only 30% of nurses can correctly identify the 4th intercostal space.
- Medical students often receive minimal hands-on ECG training.
- On-the-job training varies widely between institutions.
This lack of standardization contributes to high error rates in clinical practice.
Best Practices for Teaching Leads ECG Placement
Effective training should combine theory, demonstration, and supervised practice.
- Use anatomical models and simulators for hands-on learning.
- Implement competency assessments with direct observation.
- Provide regular refresher courses and audits.
The European Society of Cardiology recommends annual ECG competency checks for all staff involved in ECG acquisition.
Certification and Quality Assurance Programs
Hospitals and clinics should establish quality assurance protocols for ECGs.
- Random audits of ECG tracings to check for placement errors.
- Feedback loops to educate technicians on common mistakes.
- Certification programs like the Certified Rhythm Analysis Technician (CRAT) improve skill retention.
Centers with formal ECG quality programs report up to 50% fewer diagnostic errors.
Legal and Ethical Implications of Incorrect Leads ECG Placement
Misplaced electrodes aren’t just a technical flaw—they can have serious legal consequences.
Malpractice Risks and Diagnostic Errors
Incorrect leads ecg placement that leads to misdiagnosis can form the basis of malpractice claims.
- Failure to diagnose acute MI due to poor ECG quality is a common litigation theme.
- Courts expect adherence to established standards of care.
- Documentation of proper technique can serve as a legal defense.
A 2019 review in The Journal of Clinical Forensic Medicine found that ECG errors contributed to 12% of cardiac-related malpractice cases.
Patient Safety and Informed Practice
Accurate leads ecg placement is a patient safety issue. Every ECG is a medical record with lasting implications.
- Patients deserve reliable diagnostics free from preventable errors.
- Transparency about limitations (e.g., difficult anatomy) should be documented.
- Healthcare providers have an ethical duty to perform procedures correctly.
“Every electrode you place is a promise of accuracy to the patient,” says ethicist Dr. Marcus Reed.
What is the most common mistake in leads ecg placement?
The most common mistake is incorrect placement of precordial leads, especially V1 and V2. Placing them above the 4th intercostal space can mimic anterior myocardial infarction. Another frequent error is swapping the right and left arm electrodes, which reverses lead I and can suggest dextrocardia.
How can I ensure accurate V4 placement?
To ensure accurate V4 placement, locate the 5th intercostal space at the midclavicular line. Start by finding the angle of Louis (sternal angle), slide laterally to the 2nd intercostal space, then count down to the 4th and 5th spaces. Palpate each rib carefully, as visual estimation is often inaccurate, especially in obese patients.
Should chest leads be placed on breast tissue in women?
No, chest leads should not be placed on breast tissue. V3–V6 must be positioned on the chest wall beneath the breast to ensure accurate electrical signal detection. Lifting the breast to place the electrode on the underlying chest wall is the correct technique and prevents waveform distortion.
Can technology prevent leads ecg placement errors?
Yes, emerging technologies like placement templates, real-time impedance monitoring, and augmented reality apps can significantly reduce errors. While not a substitute for training, these tools provide valuable feedback and standardization, especially in high-pressure environments.
How often should healthcare providers be retrained in ECG placement?
Providers should receive refresher training at least annually. Regular competency assessments, audits, and feedback are essential to maintain high standards. Institutions with ongoing education programs report fewer placement errors and higher diagnostic accuracy.
Mastering leads ecg placement is not just a technical skill—it’s a cornerstone of accurate cardiac diagnosis. From understanding anatomical landmarks to leveraging modern technology, every step in the process impacts patient outcomes. By avoiding common errors, adapting to special populations, investing in training, and embracing quality assurance, healthcare providers can ensure every ECG tells the true story of the heart. In a world where milliseconds matter, precision in leads ecg placement can mean the difference between life and death.
Further Reading: